
Diabetes Mellitus, a problem sneaking up on us.
January 7, 2016 - Toshi Shiina, James Ziomek, MD, Mary Beugelsdijk, RN

Toshi Shiina is a premedical student at UNM-LA. He has noticed that so many patients are coping with diabetes, mostly type 2. By interviewing diabetes educators and from literature search, he learned that benefits of efforts toward prevention of the disease extend beyond diabetes. He wanted to share his findings with the community and wrote the article working with Dr. James Ziomek, MD and Mary Beugelsdijk, RN at the primary care clinic in Los Alamos.
We are facing a diabetes epidemic. The CDC reported that, in 2014, more than 29 million Americans (about one in 11 people) had diabetes a 10% increase from 2010. The concerning fact is that one in four people with diabetes do not know that they have it. [1] While scientific research is still in progress, we know that certain groups of people are known to be at higher risk of having diabetes. The known risk factors for diabetes which we cannot control are: age, genetics, race, and history of diabetes during pregnancy. On the other hand, the risk factors that we can work on are: being over-weight, high cholesterol level, smoking, high blood pressure, and physical inactivity. [2] Therefore, we can take preventive measures to reduce the risk of developing diabetes.
The Human Body
In order to understand what diabetes is, let us take a brief tour through our body at the tiny cellular level. A cell is the working unit of the body. Muscle cells use energy to contract and enable us to move, brain cells make us see and feel and control muscle movement. Heart muscle cells also use energy to pump blood through the network of blood vessels throughout the body. Cells mainly use glucose, the breakdown product of foods we eat (mostly carbohydrates), for energy to maintain life with the help of oxygen we breathe in. We breathe out the waste product, carbon dioxide. (That's how we lose carbon particles in carbohydrates after harvesting energy from foods.) Blood carries needed nutrients and oxygen to other cells so that they can do their work. The kidneys are constantly filtering blood to maintain chemical balance and blood pressure. However blood is not a storage unit. Glucose molecules must enter cells to be processed for energy. Excess glucose molecules are converted into glycogen and stored in the liver and muscles. If even more glucose molecules are available, they are converted into fat and stored under the skin and also around the internal organs as visceral fat.
Glucose Uptake
After a meal, the circulating blood glucose level (BGL) rises. Because glucose molecules are sticky, they cannot freely cross the cell membrane. It takes a special key to open the glucose gates. This key is insulin and the gates are protein molecules. Lets take a close look at the mechanism of how the gates operates. Figure 1 shows the series of events following the rise of BGL. [3]
Step 1: Elevated BGL stimulates the pancreas to release insulin into the blood stream. Insulin is created by the beta cells of the pancreas.
Step 2: Insulin binds to the insulin receptor of a cell.
Step 3: This action triggers the cascade of chemical reactions inside the cell.
Step 4: As a result, glucose transporter protein (GLUT4) is released from the vesicle. GLUT4 travels into the cell membrane—the glucose gate is open.
Step 5: Glucose is out of the blood stream and can enter the cell.
Step 6: Once inside, the cell processes glucose to harvest energy and create fat and cholesterol molecules. (Surprise!)
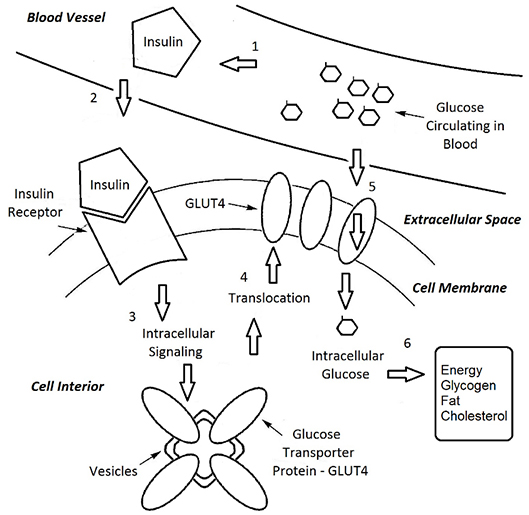
Figure 1. Chemical events following the rise in blood glucose level (BGL)
Types of Diabetes Mellitus
Diabetes mellitus (DM), commonly known as diabetes, is the disease where this glucose transportation mechanism does not work. There are mainly three types of DM:
Type 1 is caused by the loss of insulin secretion from the pancreas despite increase of BGL. This occurs when the bodys own immune cells attack the beta cells in the pancreas (autoimmune disease). Since insulin is not available to initiate the translocation of GLUT4 transporter into cell membrane, the glucose gate does not open—no key.
Type 2 is caused by the insensitivity of the insulin receptors despite presence of glucose and insulin in the blood stream (insulin resistance) and/or insufficient production of insulin. When insulin resistance develops, insulin receptors do not respond well to the increased level of glucose and insulin in blood the key does not unlock the gate. Whether type I or type II, high concentration of glucose remains in blood.
The third type is specific to pregnant females typically in the second half of pregnancy. The mechanism of gestational diabetes (GDM) is similar to Type II DM caused by the loss of sensitivity to insulin. Because gestational diabetes is associated with pregnancy, GDM may resolve after delivery of the baby. However, the baby may have a seizure upon delivery. This is because the mothers high BGL keeps the babys BGL and insulin levels high in the womb. When the umbilical cord is cut, the baby loses the glucose supply all of a sudden while his/her insulin level remains high. This causes the babys BGL to drop to a dangerous level to the brain causing a seizure. Furthermore, women who had GDM during pregnancy have higher chance to develop type 2 diabetes later in life.
Whatever the type may be, the danger of diabetes is high concentration of glucose in blood. Glucose molecules attach themselves to inside walls of blood vessels and cause micro-injuries. [4] The blood vessels in the retina, the back of the eye where the vision sensor nerves cells lie, are especially vulnerable. Some capillaries supplying blood to these nerves close off while neighboring capillaries enlarge and become leaky. Cutoff of blood supply and leaked deposits cause injury to the retina—retinopathy. Diabetic retinopathy is the leading cause of blindness in developed countries. [5] The leaky blood vessels also cause the kidneys to lose their blood filtering ability nephropathy. Glucose, proteins, and water are lost in urine. Frequent urination and dehydration would follow. If untreated, nephropathy can progress into kidney failure. A patient with kidney failure requires a transplant or a machine to filter blood regularly (dialysis). [6] Diabetes is ultimately a vascular disease, but the damage can extend to nerves causing loss of sensation in feet and hands as well as erectile dysfunction—neuropathy.
Type 1 diabetes is an autoimmune disease and can progress very quickly. The beta cells in the pancreas may stop creating insulin in a matter of weeks. On the other hand, insulin resistance in type 2 DM develops very slowly and unnoticeably. No wonder one in four people are not even aware of having type 2 DM. This is the real danger of type 2 DM. You may gradually notice subtle signs and symptoms such as frequent urination, hunger despite having a meal, depression, and/or chronic fatigue. But when untreated, chronic high blood glucose level can damage blood vessels and cause a heart attack or a stroke. In fact, doctors in Finland studied more than 2,400 people over seven years and reported that the chance of having a heart attack for a diabetic patient is as high as someone without diabetes who has already had one heart attack. [7]
The good news is that we can counterstrike the development of type 2 diabetes by making small changes to reduce risk factors in our daily life. [8]
- Weight loss: We must first determine the target weight to lose. Checking your body mass index (BMI) is a good start. BMI is defined by the formula: BMI=(weight in lb) x 703 / (height in inches)2. The National Diabetes Education Program has a table of At-Risk BMI. [2] Your target weight should guide your weight loss plan.
- Cholesterol: Although the body creates most of its cholesterol, dietary intake of cholesterol is known to raise the level of bad cholesterol in blood. The American Diabetes Association has useful information about healthful food choices at http://www.diabetes.org.
- Smoking: Quitting smoking has immediate benefits. However, it may be hard. Fortunately there is a public program that supports your effort to quit smoking for free. Call 1-800-QUITNOW or visit https://www.quitnow.net/newmexico/ and they will provide free therapy products (nicotine patches, gum, and medication) and personally coach you.
- Exercise: The NM Department of Health encourages getting physically active by monitoring the number of steps you take every day with a pedometer. If you are on Medicaid, Centennial Rewards program will challenge you and reward you for your progress. Also, adding 30 minutes of a little harder exercise three times a week will lower your blood pressure. You can add small weight lifting while taking a brisk walk on your favorite trail or while walking a dog.
Diabetes, especially type 2 DM, may be a ghost-like disease that can sneak up on you, but we can keep it away by making small changes in our daily routine toward healthful lifestyle. Furthermore, starting to reduce the risk factors for diabetes now doubles as prevention of heart disease. Lets get started!
[References]
[1] Centers for Disease Control and Prevention (CDC), Diabetes Latest
[2] National Diabetes Education Program, Diabetes Risk Factors
[3] Rosenthal, M.D. et al. Medical Biochemistry: Human metabolism in health and disease. John Wiley & Sons, Inc. 2009
[4] Milne R., et al. Advanced Glycation End Products and Diabetic Retinopathy. Amino Acids. 2013 Jun; 44(6):1397-1407
[5] Cunha-Vaz, J.G. Pathophysiology of Diabetic Retinopathy. British Journal of Ophthalmology 1978, 62:351-355
[6] American Diabetes Association, How Does Diabetes Cause Kidney Disease?
[7] Haffner, S.M. et al. Mortality from Coronary Heart Disease in Subjects with Type 2 Diabetes and in Nondiabetic Subjects with and without Prior Myocardial Infarction. The New England Journal of Medicine 1998, 339:229-234
[8] Wisneski, J. MD, Private conversation
